Abstract
Introduction: Chronic lymphocytic leukemia (CLL) is the most frequently diagnosed hematologic cancer, with many patients diagnosed at a later stage in life and typically with comorbidities that often complicate CLL management. Atrial fibrillation (AF) is the most common arrhythmia in the United States and is associated with high hospitalization and mortality rates. While the relationship between CLL and AF has been reported, there is limited real-world evidence on the clinical and economic impact of AF in CLL patients. The objectives of this study were to examine the impact of AF on cardiovascular (stroke, bleeding events, heart failure) and economic (costs and healthcare resource utilization [HRU]) outcomes among patients with CLL.
Methods: This retrospective observational study used the IBM MarketScan Research Databases in Treatment Pathways that includes at least a 10-million sample of the commercial and Medicare supplemental claims database. Patients who were at least 18 years, diagnosed with CLL (identified by ICD-9/ICD-10) and continuously enrolled from January 2009 to July 2020 were included. CLL patients were followed up for one year after their first CLL diagnosis date to examine the incidence of AF. Cardiovascular outcomes were evaluated as the incidence of stroke, bleeding events, and heart failure among the CLL patients with and without AF. Costs and HRU were assessed following up until 1 year after the first date of AF, stroke, bleeding events, and heart failure. HRU was evaluated for outpatient, emergency room (ER), inpatient, and pharmacy visits, and by length of stay (LOS) for hospitalizations. Costs were evaluated in overall population and by HRU type. Statistical differences in clinical outcomes between patients with and without AF were compared using chi-square tests. The Mann Whitney Wilcoxon test was used to compare the medians for the HRU and cost outcomes. The associations between AF and hospitalizations as well as costs were evaluated by multivariable logistic regression and generalized linear model, respectively. Statistical significance was determined at a P-value of less than 0.05.
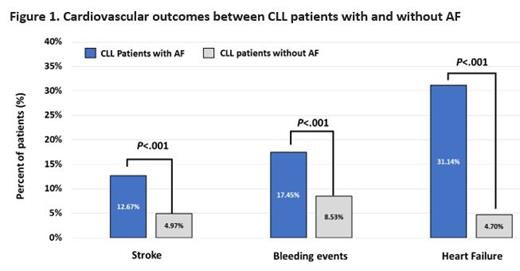
Results: Among the total of 23,756 newly diagnosed CLL patients (median age 68 years, 57.83% male) included in the study, 11% had AF within 1 year of the CLL diagnosis. CLL patients who had AF were significantly older (median age: 67 vs 82 years) and had more male patients (56.9% vs 65.1%) compared to CLL patients without AF. Significantly higher rates of stroke (12.67% vs. 4.97%), bleeding events (17.45% vs. 8.53%), and heart failure (31.14% vs. 4.70%) were observed in CLL patients with AF than those without (Figure 1). Compared to the CLL cohort without AF, adjusted regression analysis indicated that overall, CLL cohort with AF was twice as likely to be hospitalized (odds ratio [OR]=2.03) and incurred 44% higher total costs (cost ratio [CR]=1.44). Further examining the impact of AF-related cardiovascular outcomes, we observed that CLL patients with AF who developed stroke, bleeding events, and heart failure had statistically significant higher HRU (outpatient, ER, inpatient, and pharmacy visits), longer LOS, and costs (total, outpatient, pharmacy) than CLL patients without AF. After adjusting for demographic and clinical confounders, significantly higher hospitalization rates and costs were also reported in the CLL cohort who had AF with further stroke (OR=2.59; CR=1.36), bleeding events (OR=3.27; CR=2.03), and heart failure (OR=5.47; CR=2.07) compared to the CLL cohort without AF.
Conclusions: The findings of this real-world study demonstrated significantly higher hospitalizations, cardiovascular events, and economic burden incurred by CLL patients who had AF than those without. The presence of stroke, bleeding events, heart failure among CLL patients with AF further increased the HRU and costs. This study highlighted the importance of better disease management, more intentional monitoring for AF and improved CLL therapeutics with a lower risk of AF or cardiovascular toxicity to prevent or minimize the incidence of AF in CLL patients.
Mohan: BeiGene, Ltd.: Current Employment. Yang: BeiGene, Ltd.: Current Employment. Liu: BeiGene, Ltd.: Current Employment. Dick: IBM Watson Health: Current Employment. Tang: BeiGene, Ltd.: Current Employment. Chanan-Khan: Ascentage: Research Funding; Alpha2 Pharmaceuticals, NonoDev, Starton: Current holder of stock options in a privately-held company; Cellectar: Current equity holder in publicly-traded company; Alpha2 Pharmaceuticals: Patents & Royalties: Tabi; Ascentage, Starton, Cellectar, NonoDev, Alpha2 Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; BeiGene, Jansen, Ascentage: Honoraria; BieGene, Jansen, Ascentage: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal